
Healthtech Security
Article | November 29, 2023
Before we discuss the importance of telehealth and how it is changing the nursing industry in general, it is important to understand what telehealth is all about. With the advent of new-age technologies and their impact on the fast-paced, growing population, medical health is an essential department that requires special attention. One’s health is of utmost importance, and to enhance the medical facilities, we as responsible citizens and experts in this particular field must come up with novel and quick solutions to provide optimum precaution and cure. Hence, one of such technological achievements is telecommunication,s and by utilizing such a useful resource, health-related services too can be offered. Telehealth promotes the distribution of various services related to medical health through electronic devices and telecommunication technologies. What can one possibly do if he or she lives in a different country and is pushed to an emergency situation where he requires medical advice from a physician who lives in another corner of the world? Of course, through telecommunication devices, the whole process of exchanging information becomes smoother and easier. Several health-related services such as medical advice, medical care, monitoring, education, remote admissions, and intervention can be extended to a long-distance patient with the help of telehealth facilities. Hence, the contemporary picture of health and medicine has been radically improved with the introduction of these electronic telecommunication systems.
Read More

Health Technology, Digital Healthcare
Article | August 21, 2023
Embracing the AI Revolution: Transforming Digital Healthcare Software through AI-Enhanced UX Testing
The wave of demographic change sweeping the United States presents an urgent call to action for healthcare providers. According to the US Census Bureau, adults over 65 will account for a quarter of the US population by 2060, signaling a drastic shift in healthcare delivery needs. More than half a million of this demographic will be centenarians, accentuating the need for digital experiences tailored to seniors' unique needs.
Despite the rapid advancement of digital health technologies, research indicates that many senior citizens struggle to adapt. A recent study reported that 40% of adults over 65 believe their telemedicine visit was inferior to traditional in-person care, with a meager 5% finding it superior. The promise of convenience delivered by digital health is often overshadowed by the frustration associated with technical difficulties. An astounding 75% of senior citizens admit they need assistance when using new electronic devices.
Let's consider the patient portal app, a common touchpoint in the digital health journey. Despite its apparent simplicity, seniors find processes like logging in troublesome due to issues like forgotten passwords, technical bugs, or content readability. This scenario underlines the crucial need for comprehensive User Experience (UX) testing to eliminate these barriers and provide a seamless digital health experience.
The Complex Landscape of Healthcare UX Testing
The complexity of UX testing in healthcare has been exacerbated by the interplay of multiple modules, services, platforms, and vendors. Take Electronic Medical Record (EMR) systems, for instance, which undergo frequent updates, each one potentially impacting the system as a whole. Traditional manual testing methodologies are proving to be time-consuming and costly.
Though automation has revolutionized sectors from automotive to finance, the healthcare industry appears to be lagging. A study by the Health Information and Management Systems Society (HIMSS) reveals that a mere 15% of healthcare providers have adopted modern test automation platforms. Meanwhile, a significant 41% still rely on manual testing. As EMR systems grow increasingly complex and customized, this over-reliance on manual testing poses daunting challenges.
The gravity of this issue is amplified by a startling revelation from the HIMSS study - only 6% of healthcare executive leaders express confidence in their organizations' testing practices. In an increasingly digitized healthcare environment, such a low level of assurance raises substantial concerns about patient safety. Although 75% of the surveyed providers have invested in software testing to safeguard their bottom lines, nearly two-thirds confess feeling inadequately resourced in terms of time, money, and talent to meet future testing requirements. As the list of testing demands grows, QA teams are frequently stretched thin, leaving many potential user journey scenarios untested.
The Power of AI in UX Testing for Better Patient Outcomes
AI technologies hold the potential to revolutionize UX testing in healthcare.
The modern healthcare application is a labyrinth of potential user journeys - a typical mobile application model can yield over 9 billion separate scenarios. To effectively navigate this colossal testing landscape, test automation tools employing Machine Learning (ML) algorithms are critical.
By analyzing historical patterns, prioritized cases, and real-user insights, ML algorithms can auto-generate test cases and meticulously scrutinize each user interaction. This approach ensures an optimal digital experience and robust coverage of potential issues.
The HIMSS study also provides a glimmer of hope, revealing that nearly 80% of healthcare providers plan to adopt real-time testing analytics for quality assurance. AI's role becomes pivotal in augmenting the capacity of software testing teams in this scenario.
By leveraging historical patterns and prioritizing test cases, ML-powered testing tools can automate crucial tests across various platforms, devices, and operating systems. This symbiosis of human expertise and AI not only bolsters productivity but enables comprehensive testing coverage within tight time constraints.
The Future of Healthcare Software UX Testing
The path to perfecting a patient’s digital journey is fraught with challenges.
Healthcare organizations venturing into automated software testing or contemplating in-house tool replacement must stay abreast of evolving healthcare testing requirements. This understanding is key when evaluating automation vendors against the backdrop of regulatory standards. Opting for a technology-agnostic solution ensures extensive test coverage, boosts efficiency, and guarantees longevity as technologies advance. Introducing your software QA teams to user-friendly, low/no-code test automation tools can simplify the onboarding process and fosters better collaboration with Dev teams and business testers.
As we stand at the precipice of this transformative period in healthcare, it's clear that the AI revolution holds the key to unlocking the future of digital healthcare UX testing. By harnessing AI's potential, healthcare providers can ensure a user-friendly, seamless digital experience for the fastest-growing demographic, setting new industry standards in the process.
Read More
Health Technology, Digital Healthcare
Article | August 16, 2023
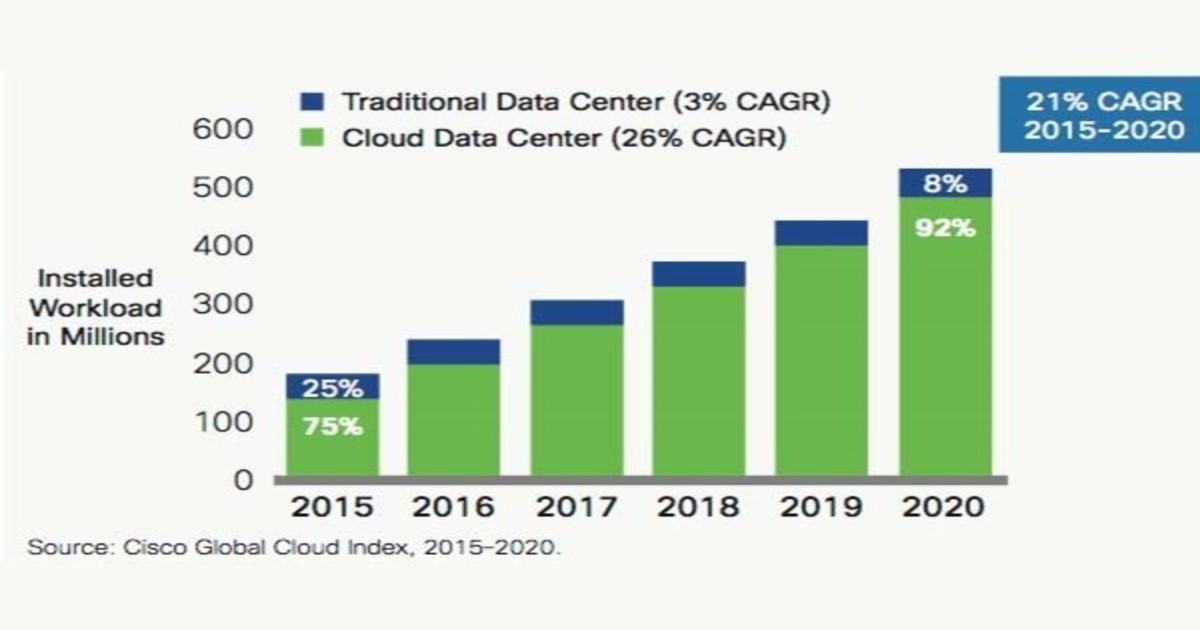
Over the past twenty-five years most businesses have been revolutionized by the easy availability of cloud and mobile-based computing systems. These technologies have placed power and access into the hands of employees and customers, which in turn has created huge shifts in how transactions get done. Now the companies with the highest market value are both the drivers of and beneficiaries of this transition, notably Apple, Facebook, Amazon and Alphabet (Google), as well as their international rivals like Samsung, Baidu, Tencent and Alibaba. Everyone uses their products every day, and the impact on our lives have been remarkable. Of course, this also impacts how businesses of all types are organized. Underpinning this transformation has been a change from enterprise-specific software to generic cloud-based services—sometimes called SMAC (Social/Sensors/Mobile/Analytics/Cloud). Applications such as data storage, sales management, email and the hardware they ran on were put into enterprises during the 80s and 90s in the client-server era (dominated by Intel and Microsoft). These have now migrated to cloud-based, on-demand services.
Read More

Health Technology, Digital Healthcare
Article | September 7, 2023
Unlock EHR interoperability solutions with this article. Discover how healthcare overcomes EHR interoperability challenges to facilitate seamless information sharing for better clinical decisions.
1. Exploring Hurdles in EHR Interoperability
2. Addressing EHR Interoperability Challenges: Mapping Effective Paths
2.1 Upgrading from Outdated Legacy Systems
2.2 Managing Inconsistent Information Across Multiple Sources
2.3 Overcoming Organizational Resistance to Sharing Data
2.4 Balancing Security and Consent
2.5 Harmonizing Data Standards Across Diverse Software Systems
2.6 Optimizing Training Resources for EHR Interoperability
2.7 Strategizing Costs for Specialist-driven Interoperability Management
2.8 Navigating Budget Constraints in EHR Interoperability
2.9 Unifying Patient Identification Standards Across HIEs
2.10 Advancing Allergy Management to Enhance Patient Care
3. Embracing Interoperability for a Connected Healthcare Future
1.Exploring Hurdles in EHR Interoperability
Despite significant efforts and investments in health information systems and technology, coupled with many years of widespread availability, the full benefits of electronic health records (EHRs) still need to be realized. The reality is that most physicians continue to rely on faxing and mailing patient records, just as they did a decade ago. Numerous government-certified EHR products are being used, each utilizing distinct clinical terminologies, technical specifications, and functional capabilities. These differences make it challenging to establish a unified standard interoperability format for data sharing. Interestingly, even EHR systems built on the same platform might not be interoperable, as they are frequently highly customized to an organization’s specific workflow and preferences. Given these circumstances, the article examines ten challenges and their corresponding EHR interoperability solutions to enhance patient care.
2.Addressing EHR Interoperability Challenges: Mapping Effective Paths
The primary goal of healthcare interoperability is to enable seamless sharing of health-related information between healthcare providers and patients, aiding in clinical decision-making. Here are several challenges to accomplishing this aim, along with their corresponding interoperability solutions:
2. 1 Upgrading from Outdated Legacy Systems
One of the significant challenges in achieving EHR interoperability is the need to transition from outdated legacy systems. Many healthcare facilities still rely on older, proprietary EHR systems that need more compatibility and standards to communicate seamlessly with modern, interconnected healthcare networks. These legacy systems often need more data exchange capabilities, leading to inefficiencies, data inconsistencies, and barriers to collaborative patient care. The intricate process of upgrading or replacing these systems while ensuring data integrity and continuity of care poses a considerable obstacle to achieving comprehensive EHR interoperability.
Healthcare institutions need to implement a strategic and phased approach to address this challenge. This involves assessing the existing EHR, identifying interoperability gaps, and selecting modern healthcare interoperability solutions that adhere to industry standards, such as Fast Healthcare Interoperability Resources (HL7 FHIR) and open APIs. A well-defined migration plan should be developed, including data migration, new system integration, and staff training. Collaboration with EHR vendors, IT experts, and clinical stakeholders is crucial to ensuring a smooth transition.
2.2 Managing Inconsistent Information Across Multiple Sources
As patients move through different healthcare settings and encounter various medical professionals, their health information becomes distributed across multiple sources, leading to discrepancies, duplications, and variations in data. This inconsistency can compromise patient safety, treatment accuracy, and healthcare quality. Furthermore, different institutions' varying data formats, coding systems, and documentation practices exacerbate the challenge of creating a unified and accurate patient record.
A potential solution to this challenge involves developing and adopting standardized data exchange protocols. By implementing common data standards and practices, healthcare providers can ensure that patient information is accurately represented and uniformly understood across different systems. In addition, robust data validation processes and reconciliation algorithms can help identify and rectify inconsistencies during data integration. Moreover, creating a centralized patient identity management system that links various patient records to a single, accurate identity can significantly mitigate the issue of duplicated or mismatched information.
2.3 Overcoming Organizational Resistance to Sharing Data
This EHR interoperability challenge pertains to the reluctance of healthcare institutions, clinics, and providers to readily exchange patient information and medical records due to concerns over data privacy, competitive advantage, and operational complexities. This resistance often leads to fragmented patient care, hindered medical research, and compromised clinical decision-making.
Addressing this challenge necessitates the establishment of clear data-sharing protocols, robust privacy safeguards, and incentivized collaboration. By fostering a culture of trust, emphasizing the collective benefits of data exchange, and implementing interoperability standards, the healthcare ecosystem can encourage reluctant organizations to actively share essential patient data, ultimately leading to improved patient outcomes and more efficient healthcare delivery.
2.4 Balancing Security and Consent
This challenge in EHR interoperability revolves around the delicate equilibrium between ensuring patient data security and privacy while enabling the seamless sharing of EHRs across different healthcare systems. Striking the right balance involves addressing concerns about unauthorized access, data breaches, and patient consent preferences. While robust security measures are necessary to safeguard sensitive health information, overly stringent restrictions can hinder the efficient exchange of vital medical data, potentially impeding timely and informed patient care, medical research, and healthcare system efficiency.
Potential EHR interoperability solutions to this challenge include implementing a layered security and consent management approach. This involves combining strong encryption, authentication protocols, and access controls to ensure the integrity and confidentiality of EHRs. Moreover, the adoption of standardized and granular consent mechanisms empowers patients to regulate both access to their data and the purposes for which it can be accessed. An integrated framework that employs advanced technologies like blockchain for secure audit trails and data-sharing logs can enhance transparency and accountability. Furthermore, patient education and awareness campaigns can empower individuals to make informed data-sharing decisions, fostering a collaborative environment where security, consent, and interoperability coexist harmoniously.
2.5 Harmonizing Data Standards Across Diverse Software Systems
This challenge encompasses integrating and exchanging medical data across various software platforms and applications used within the healthcare industry. To tackle this challenge, a comprehensive solution includes the widespread adoption and adherence to standardized data formats, coding conventions, and communication protocols by developers, healthcare organizations, and EHR integration software.
To address this challenge, a comprehensive solution involves the establishment of standardized data formats, coding conventions, and communication protocols widely adopted and adhered to by EHR software developers and healthcare organizations. This could be achieved through industry collaboration, government regulations, and incentives for adopting interoperability standards. Additionally, implementing APIs that translate and map data between different formats can help bridge the gap between diverse software systems.
2.6 Optimizing Training Resources for EHR Interoperability
This hurdle involves preparing healthcare professionals, IT staff, and other stakeholders to effectively navigate and implement interoperable EHR systems. Ensuring that healthcare personnel possess the necessary skills and knowledge to seamlessly integrate, maintain, and utilize interconnected EHR systems amidst rapidly evolving technology and standards poses a significant hurdle. This challenge involves understanding the intricacies of interoperability protocols and grasping the broader context of data security, patient privacy, and efficient data exchange among diverse healthcare entities.
To address this challenge, developing comprehensive and up-to-date training programs that cover both technical aspects (interoperability standards, APIs, and data formats) and practical considerations (security protocols, data governance) is crucial. Collaborations with vendors, industry experts, and academia can ensure the training content remains aligned and updated with current EHR trends. Integrating EHR interoperability education into medical and IT curricula can also lay a foundation for future professionals. Continuous learning opportunities, including EHR analytics courses, certifications, and knowledge-sharing platforms, can further bolster the continual development of skills and knowledge exchange. This process cultivates a skilled workforce capable of fully leveraging EHR interoperability while upholding the integrity and privacy of patient data.
2.7 Strategizing Costs for Specialist-driven Interoperability Management
This challenge pertains to the complex and costly task of ensuring seamless data exchange among diverse EHR systems, mainly when managed by specialists with domain-specific knowledge. These specialists play a crucial role in tailoring EHR interoperability solutions to the unique needs of their medical domains. Still, the financial implications of such endeavors can be substantial, involving customization, integration, and maintenance expenses.
Finding an effective solution requires a multi-faceted approach involving standardized interoperability frameworks, modular system design, strategic resource allocation, and collaborative partnerships among EHR vendors, healthcare institutions, and specialists. By optimizing the balance between customization and standardization and leveraging technological advances like APIs and cloud computing, healthcare ecosystems can mitigate costs while achieving efficient and secure data exchange that benefits patients and healthcare providers.
2.8 Navigating Budget Constraints in EHR Interoperability
This issue relates to healthcare organizations' significant financial limitations when striving to establish seamless EHR data exchange across disparate systems. As healthcare entities aim to enhance patient care coordination and data accessibility, the cost of implementing and maintaining interoperable EHR systems becomes a substantial hurdle. This challenge necessitates a delicate balance between allocating resources for EHR integration, customization, and ongoing maintenance while ensuring that patient data remains secure and accessible to authorized stakeholders.
A possible avenue to deal with the budget constraints in EHR interoperability is the strategic adoption of open-source frameworks. By leveraging open-source solutions, healthcare organizations can reduce licensing fees and development costs associated with proprietary systems, allowing them to allocate resources more efficiently. Additionally, collaborating with industry consortia and governmental initiatives that promote standardized data exchange protocols can foster economies of scale, streamlining the implementation process. Moreover, investing in cloud-based technologies can offer scalable and cost-effective data storage and sharing infrastructure.
2.9 Unifying Patient Identification Standards Across HIEs
The crux of this issue involves the need for consistent patient identification methods across different healthcare systems and data-sharing networks. This inconsistency results in errors, data duplication, and compromised patient safety as information is exchanged between entities. Without a standardized patient identification system, accurate matching of patient records becomes a complex endeavor, hindering the seamless exchange of EHRs and undermining the potential benefits of interoperability.
To address this challenge, a comprehensive solution involves establishing and adopting a universally recognized patient identification standard that spans all participating HIEs. This standard could include using unique patient identifiers or a combination of demographic, biometric, and cryptographic identifiers to ensure accurate and secure patient matching. Additionally, implementing advanced data governance practices, strong privacy protections, and robust data validation algorithms would enhance the accuracy and security of patient identification. Collaboration between healthcare organizations, government agencies, and technology experts is crucial to developing and implementing this standardized approach, fostering a more interconnected and effective healthcare ecosystem while safeguarding patient privacy and data integrity.
2.10 Advancing Allergy Management to Enhance Patient Care
Healthcare providers need help seamlessly sharing allergy-related patient data across different EHR platforms, hindering comprehensive patient care. This lack of interoperability leads to fragmented information, potential medication errors, and compromised treatment decisions, ultimately impacting patient safety and outcomes.
One viable solution for addressing this challenge is to establish standardized data exchange protocols alongside a unified health information exchange framework. Implementing FHIR standards can enable the consistent and secure sharing of allergy information among EHR systems. Additionally, incentivizing healthcare organizations to adopt these interoperability EHR standards and invest in compatible technologies will promote a cohesive ecosystem where allergy data can be accurately and swiftly exchanged. Collaborative efforts among EHR vendors, healthcare providers, and regulatory bodies are essential to ensure the seamless flow of allergy-related information, resulting in enhanced patient care, reduced medical errors, and improved healthcare efficiency.
3.Embracing Interoperability for a Connected Healthcare Future
With the goal of a cohesive healthcare future in mind, the value of embracing interoperability is immeasurable. This article highlights the essential role of interoperability in overcoming the challenges posed by fragmented data and improving patient outcomes. As healthcare systems continue to develop, the smooth exchange of EHRs becomes crucial, fostering collaboration among diverse stakeholders and facilitating well-informed decision-making. By creating an environment in which EHRs can seamlessly communicate, healthcare providers have the potential to offer more comprehensive, patient-centered care, minimize duplication, and expedite both diagnoses and treatments. Although achieving an interoperable healthcare ecosystem may involve complexity, the benefits of efficiency, precision, and overall quality of care underscore its necessity as a transformative journey.
Read More